The kidneys filter blood, remove waste through urine, balance minerals, maintain fluid balance, and produce hormones. When you have kidney disease, the kidney function declines such that the kidneys could no longer filter waste materials in the body properly. Fluid and waste can build up in the blood, which could result in serious complications.

Following a kidney diet can help slow the progression of kidney disease and protect the kidney from further damage. Besides eating nutritious foods that are gentle on the kidneys, a renal diet also involves limiting certain food sources that can aggravate your condition. A renal diet also ensures you get the right balance of minerals, vitamins, calories, protein, sodium, phosphorus, etc.
CKD Dietary restrictions
Dietary restrictions depend on the stage of kidney disease. If you are in the early stages, you will have different limits compared to people at the end stage of renal disease or in dialysis. As your disease gets worse, you need to be more careful about what you consume to avoid straining your kidneys. Talk to your doctor about diet restrictions, or ask a renal dietitian for a personalized meal plan.

Early stages of CKD
People in the early stages of CKD don’t usually show symptoms and may only be diagnosed through urine or blood test. Their Glomerular Filtration Rate (GFR) at a normal or higher level greater than 90 ml/min. Since kidneys still perform their function even when they’re not at their 100 percent capacity, most people are unaware they have stage 1 CKD. They typically find out they are in stage 1 if they were being tested for a health condition that is a CKD risk factor such as diabetes and high blood pressure.
The waste accumulation in the early stages may be gradual, such that the body gets accustomed to having those waste materials in the blood. After months or years, your kidney disease may progress to permanent kidney failure that needs regular dialysis or kidney transplant, if left untreated or not managed early on.
As the kidneys are still functioning well during the early stages, the goal of a renal diet in this phase is to preserve kidney function, manage blood pressure and blood sugar, especially if you have diabetes. A dietitian may recommend Dietary Approaches to Stop Hypertension (DASH) diet to manage blood pressure and lower the risk of cardiovascular disease and formation of kidney stones. DASH diet is recognized by healthcare professionals as a treatment for heart disease, blood pressure, and possibly for CKD patients suffering from hypertension. It limits daily sodium intake to 2,300 milligrams (mg) at most, and protein intake to 18% of a person’s total calories. Healthy adults are recommended to have no more than 2300 mg per day of sodium, while CKD patients should keep it between 750 mg - 2000 mg per day. Ask your doctor or dietitian about how much sodium you need per day.
People on dialysis aren’t advised to follow a DASH diet, as they have different dietary requirements.

When you are in the early stages of CKD, risk factors such as high blood pressure, high blood sugar, proteinuria, high cholesterol, and chronic inflammation can be managed by following a renal diet.

High Blood Pressure
The World Health Organization shares that the “restriction of sodium intake to less than 2.3 g a day of sodium corresponding to 5.8 g of salt (or 100 mmol) is one of the most cost-effective measures to improve public health.” Decreasing your intake of food high in sodium helps manage blood pressure. Foods high in sodium include processed food, fast food, cured foods, canned goods, and cured foods. You also need to steer clear of salt substitutes as they can spike your potassium level, which can affect your kidney disease.
Understanding nutrition information on food labels allows you to make smart food choices. Too much sodium in the body can cause edema or swelling of the face, hands, legs, or feet. Besides higher blood pressure, you may also experience difficulty in breathing or shortness of breath. Click this link to know more about managing high blood pressure when you have CKD.
Hyperglycemia (high blood sugar)
Too much sugar in the blood, hyperglycemia, is associated with diabetes. It can cause rapid heartbeat, excessive hunger, vomiting, vision problems, and other symptoms. Hyperglycemia takes place when the body has too little insulin (the hormone that delivers sugar or glucose into the blood) or if your body can’t use insulin well.
Hyperglycemia is blood sugar that is greater than 125 mg/dL (milligrams per deciliter) while a person with fasting blood glucose greater than 125 mg/dL has diabetes. Uncontrolled diabetes speeds up kidney function loss and contributes to cardiovascular disease and other diabetes complications. Carbohydrate counting can help you stay within set carbohydrate targets. Opt for high fiber and low sugar foods. Click this link to know more about sugar substitutes.
Proteinuria
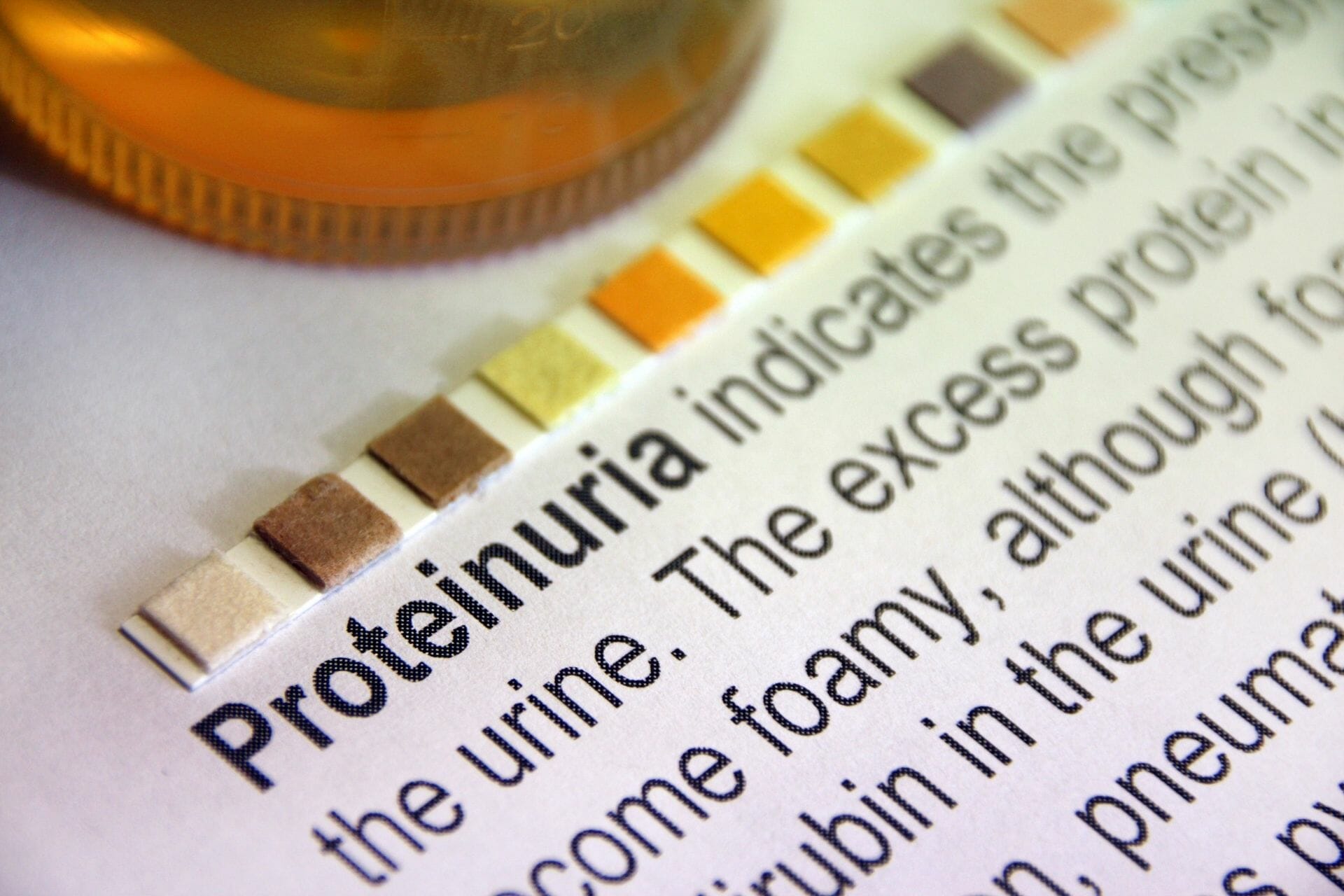
When you have CKD, you are at risk of proteinuria or protein in the urine due to losses through the kidneys. Decreasing protein intake while you are still at the early stage of CKD may help slow down kidney function loss.
High Cholesterol
Dyslipidemia is the imbalance of lipids like triglycerides, high-density lipoprotein, and low-density lipoprotein cholesterol. You can manage high levels of cholesterol by consuming healthy fats instead of trans fats, saturated fats, and animal fats. Great sources from olive or canola oil, nuts, and seeds. Meanwhile, consider limiting your consumption of foods rich in trans fat such as fried foods, dairy, non-dairy creamers, crackers, pizza, canned frosting, etc.
ESRD Diet Restrictions
End-stage renal disease (ESRD) is the end result of many forms of CKD, characterized by severely limited kidney function. At this point, the kidneys are insufficient to maintain a life where most patients are required renal replacement therapy through hemodialysis, peritoneal dialysis, or kidney transplantation.
The ESRD diet considers lab results, nutritional status, plans for treatment (transplant, dialysis, or no treatment). Eating is becoming challenging at this point due to uremia. Uremia is an increased blood urea concentration that causes breathlessness, nausea, anorexia, weight loss, lethargy, seizures, coma, etc. Generally, once CKD has progressed to ESRD, it is irreversible. The goal of the treatment is to treat complications and replace kidney function through dialysis or kidney transplant.

Plenty of CKD patients is malnourished, which put them at increased risk of mortality. Accumulation of toxins, chronic inflammation, dialysis procedure, and comorbid conditions may affect their appetite. The goal of the ESRD diet is to prevent malnutrition, as it can reduce the risk of hospitalization and even death before starting renal replacement treatment or undergoing a kidney transplant.
Non-Dialysis ESRD Diet Restrictions
Restricting protein can help minimize waste accumulation in the blood and manage uremia. However, following a low-protein diet with appetite loss can result in malnutrition. When you are at ESRD, the National Kidney Foundation of Hawaii, Inc. suggests limiting protein to 0.55-0.60 grams per kilogram of body weight to delay decline in kidney function.
Renal Replacement Diet Restrictions
The kidneys can no longer get rid of waste materials in ESRD, in this case, renal replacement therapy helps some of the work that your kidneys did when they were healthy. Nevertheless, dialysis doesn’t work as well as healthy kidneys and cannot perform everything that healthy kidneys do. Between dialysis treatments, some waste and fluid may still accumulate in the blood, which can cause heart and bone problems. You must monitor the amounts of fluid and specific nutrients you consume to keep waste and fluid buildup in your blood.
As dialysis removes protein from the blood, you may need to increase your protein consumption to make up for the protein you’ll lose through dialysis. Your protein intake is dependent on your kidney function, body size, and nutritional status, which is why it’s best to talk to your healthcare provider about your recommended protein intake per day. Moreover, your nephrologist may monitor your sodium, potassium, phosphorus, and protein levels to ensure your diet matches your nutritional requirements.
Hemodialysis Diet
You will likely need to limit your protein, potassium, sodium, phosphorus, and fluids intake strictly if you are on hemodialysis treatments thrice (3x) a week. There is more time between sessions for waste and fluid to build up, as the blood is being cleaned only thrice a week. However, if you do at-home hemodialysis daily, you may follow a less strict diet.
Peritoneal Diet
On the other hand, if you are receiving peritoneal dialysis treatment, you may consume slightly more phosphorus, potassium, sodium, and fluid compared to when you’re receiving hemodialysis. You may be also required to increase your protein intake as PD works all day and night to remove waste and fluid in the blood to prevent build-up in your blood as it does between hemodialysis treatments.
People with diabetes and receiving dialysis
Diabetes has unique dietary requirements such that you need to limit specific nutrients while controlling your blood sugar. Note that peritoneal dialysis solution has dextrose in it. As a type of sugar, you need to consider the dextrose content in your peritoneal dialysis solution if you have diabetes as extra sugar. Discuss with your healthcare provider if you have concerns about managing your glucose if you receive peritoneal dialysis.

The Bottomline
Following a kidney-friendly diet can sound restrictive and overwhelming initially. However, your nephrologist and renal dietitian can help you embrace a healthy lifestyle and eating habits that are attuned to your dietary and nutritional requirements. You also need to discuss your dietary requirements with your family and loved ones, so they can help and support you with your diet. Embracing a renal diet allows you to have more control over how you feel. At best, it would help slow down the progression of your kidney disease and protect your kidneys from further damage A renal diet encourages you to be more aware of what you put in your body and avoid further burden on your compromised kidneys, which could carry you through to attain your health goals as a CKD patient.

